It’s Time For A Revolution in Throwing Rehab
One night last winter my friend, Alan Jaeger called me with a major concern about the current state of UCL reconstruction post-operative rehabilitation and throwing protocols. We talked for about an hour, and the discussion ignited a thought eruption that had been smoldering in my head for over 10 years.

At the Florida Baseball ARMory we train and develop high-caliber throwing athletes, improving velocity, command, secondary stuff, and arm health. This past summer, 161 high school and college baseball players made the trek to Lakeland, FL to begin their own relentless pursuit of excellence in our Complete Game Summer Training Program, They trained up to five hours per day, five days per week and they stayed anywhere from 2-10 weeks. The energy, intensity, and focus was palpable and he the results were incredible.
It has been our honor to assist players in achieving performance levels they have heretofore only dreamed of. Our hyper-individualization of multifaceted training is the keystone of our process. At the ARMory, we frequently advise our students, “If you find yourself involved in a training experience where everyone in the program does the same thing all the time, RUN!!! If you “google return to throwing programs” the first 10 pages (notice I said “pages”, not “articles).”
I believe it’s time for UCL rehabilitation to undergo a radical change.
At the core of any rehabilitation process are 2 fundamental laws of physiology:
1) Wolff’s Law states that bone grows and remodels in response to the forces that are placed upon it in a healthy person.
2) Davis’s Law is a physiological principle (the corollary to Wolff’s Law) stating that soft tissue continually remodels and heals according to how they are mechanically stressed.
Rehab Protocols Must Adhere To Known Principles of Tissue Organization
Many esteemed members of the medical profession appear to ascribe to the idea that nearly all throwing injuries are due to “overuse” and that “you only have so many bullets in the gun, so you have to save them.” Those who do so are either denying or ignoring Davis’s law which applies to all human connective tissue that has a blood supply. While the UCL, Labrum, and rotator cuff aren’t the most highly vascularized tissues, they do receive some blood flow, and therefore under the right conditions, they are capable of remodeling themselves to resist the stresses under which they are placed.
I’ve had the privilege of scrubbing in for surgery with Dr. Koko Eaton, the Tampa Bay Rays team physician, who during a few different UCL reconstructions lifted the fragment of a torn UCL and said, “look at how thick this ligament has gotten. This injury has been coming on for a long time.” My thoughts immediately turned to Davis’s law. “That confirms it,” I thought. “A thickened ligament indicates that it was attempting to remodel itself to resist the stress.” Unfortunately for this guy, it wasn’t able to remodel fast enough to keep up with the pace of the stress.
During one particular surgery, Dr. Eaton had harvested an exceptionally long portion of the patient’s palmaris longus tendon (to be used as the replacement UCL). He drilled four holes in the in the bone and wrapped the tendon through in 3 full figure 8’s. Next, Dr. Eaton tested the stability of the graft with an aggressive valgus stress maneuver. I mean, he really popped it hard. I almost fell over from the startle reflex. I was shocked. In physical therapy, we had always treated our post-UCLR patients with kid gloves, gingerly handling the elbow and avoiding all valgus stress. After I had regained my senses, I said, “Wow. That looks like a pretty stable repair (I know. Brilliant, right?).” Dr. Eaton nodded and stated, “You know, Randy. This new ligament isn’t really the main stabilizer of the elbow. It’s just the lattice for the scar tissue. As it forms around the ligament, the scar will become the primary stabilizer.” He added, “Whenever we have to go back in for a second repair, “It looks like a grenade went off in the guy’s elbow. There is just this massive blowout of scar tissue.”
Well, that really got me thinking.
In physical therapy, we’ve used the same universal UCL rehab program for as long as I can remember. A surgeon might add a few nuances, or choose a preferred brace, but early physical therapy is pretty much a one-size-fits-all approach that involves minimal motion – even bracing – for the first several days/weeks. We progress through isolated, guarded ranges of motion in unidirectional planes (flexion and extension, supination/pronation), avoiding any valgus stress for at least eight weeks. We don’t begin any movement that simulates the kinematics of throwing until at least 16 weeks post-op. During that time, the stabilizing scar is forming without any guidance. If you’re not interested in the biological processes in the body, skip the next section. If this kind of stuff interests you, here’s how the scar is formed:
The Physiology of Tissue Healing
Immediately (within seconds or minutes) after the surgery there is a brief constriction of blood vessels followed by rapid vasodilation. Vessels that were shut down are re-opened and widened as the tissue is infused with fresh blood – blood that contains many of the necessary healing agents for recovery and the ever-important undifferentiated mesenchymal cells (UMCs) that begin forming the scar. UMCs are like over-the-counter stem cells that run in the platelets of the blood. They have no real job until tissue is injured. When they receive what is assumed to be a chemical signal about tissue injury or death, they have the miraculous ability to morph themselves into whatever kind of cells they need to become to replace the injured or dead cells. UMCs are the same cells involved in the PRP (platelet-rich plasma) injection procedure that has become popular in the last 8-10 years.
After this period of vasodilation and infusion, the rate of blood flow diminishes. This increases the hydrostatic pressure which causes fluid to leak out of the blood vessels and into the surrounding tissue. The fluid that leaks out is called transudate, and it consists of fluid, scant amounts of protein, but it no intact cells. The migration of this watery fluid out of the vessels increases the viscosity of the blood. This condition is known as haemoconcentration (thickening of the blood).
If the flow slows to a crawl or even stops, endothelial cells that make up the inner lining of the blood vessels begin to die for two reasons: 1) the roughness of the blood due to increased viscosity which scrapes the cells off the inner wall, and 2) hypoxia (lack of oxygen) as they are physically separated from blood cells carrying much-needed oxygen.
When endothelial cells die or become dysfunctional, a critical process for evacuating cellular debris is disrupted, and constipation or backflow occurs. This is a primary reason we believe ice to be contraindicated immediately postoperatively. Ice causes vasoconstriction and impedes blood flow. Continued or enhanced blood flow will avoid the traffic jam that could result in permanent damage to endothelial cells and could cascade into more widespread necrosis (or cell death). For more problem with icing as a therapeutic modality, see the works of Gary Reinl, the author of Iced: The Illusionary Treatment Option.
When epithelial cells are preserved, the clean-up can begin. White blood cells (also called leukocytes) roll along the inside of the epithelial cell wall adhering transiently to form what looks like white brick pavement along the edge of the vessel wall. The white blood cells that manage to stick to the inner wall then shoot out little “pseudopods” that become what are known as polymorphs. These polymorphs lift up the endothelial barrier and squeeze through to produce holes in the membrane. At this point, white blood cells migrate through the holes and secrete a protein that locks on to a corresponding protein on the pseudopod on the outside of the endothelial wall. The process of passing through the vessel wall is called emigration. When the protein bond is complete, emigrated white blood cells/pseudopods begin to move toward the injury site for cleanup. Remarkably, they travel against the concentration gradient, like a salmon swimming upstream, in a process known as chemotaxis. When healthy cells are injured, they release 3 chemotactic agents (C5a, C3a, and C567). These agents send a powerful signal to the white blood cells that attract them to the site of the injury. This reaction is facilitated by magnesium and calcium ions.
When the white blood cells (also known as phagocytes) arrive on the scene, they don’t strike right away. They gather in a process called aggregation, then they recognize and engulf any unwanted debris, wrapping the garbage in a well-contained cellular trash bag before being passively transported into the lymphatic system for evacuation.
The lymphatic system can be thought of like the waste management service of the body. It’s like the trash man, hauling off and disposing of unwanted garbage. But, the lymphatic system is passive. It doesn’t send trash men out to pick up the trash; it waits for the phagocytes full of dead debris to wander near the lymph nodes. As they diffuse into the lymph system, they are evacuated through the kidneys. The passive nature of the lymphatic system is why early movement and muscle pumping such as that produced by Marc Pro® electrical stimulation and the pressure gradient created by Rocket Wrap® a both valuable parts of our rehabilitation and recovery programs.

Once the clean-up is complete, the road is clear for the UMCs to do their thing. They morph into the appropriate replacement cells and, like fresh recruits on the battlefield, assume their new position.
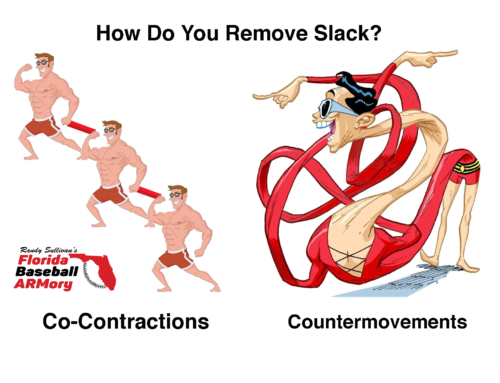
However, there is one more step they need to achieve an optimal outcome – a mechanical signal to direct their alignment. Following Davis’s Law, if we don’t provide a mechanical signal, by adding controlled stress to the new tissue, it forms in a disorganized fashion, like a plate spaghetti noodles left out in the sink all night. Disorganized tissue is unstable. Disorganized tissue is vulnerable. Disorganized tissue adheres to anything it can cling to, including, in the case of UCL reconstruction, the tendon graft that serves as the lattice for the newly forming scar.

In the current universal UCL rehabilitation protocol, we wait at least 16 weeks before we expose the elbow to any stresses that even remotely resemble the demands of actual throwing. During the entire process, in nearly every case, we fight a common enemy – scar tissue. Fearful of imparting any level of valgus load, we attempt to eliminate functional stress and try in vain to manage the scar from the outside with modalities like cross friction massage, instrument-assisted soft tissue mobilization (IASTM), and a collection of vaguely defined manual therapy techniques commonly known as “soft tissue work.” Please don’t get me wrong here, I’m not averse to these modalities, I’m certified in IASTM and use it sparingly as a pain management intervention and in cases where we might a have a gnarly, adherent scar. Nonetheless, in my opinion, those who believe we can impart order on tissue from outside of the body are sorely mistaken. That’s not the way Davis’s Law works. We might be able to break some of the superficial fibers loose, but even then, without internally activated stress created by movement, we can never achieve optimal scar tissue organization.
The Moment

When I teach physical therapy continuing education classes on UCL rehabilitation, one of the slides I post is the image of a guy looking like he’s stressed and about to vomit. I call it “the moment.” The message is that as therapists and coaches we should prepare our players for an inevitable moment that nearly every recovering UCLR experiences. It usually happens at about 7-9 months post-operation. As the player begins to ramp up his throwing program toward more game-like intensity, he/she feels that dreaded and infernal “pop”! The immediate and terrifying thought is that they’ve re-injured the elbow, but more times than not, it’s just scar tissue breaking free. After about 7-10 days, the elbow starts feeling better, and the throwing program may be resumed. Why does this occur? I would suggest that the reason we fight scar tissue like this is that we allow it to become severely disorganized during our first 16 weeks of rehab.
Could it be that the for the lucky athletes, the frightening “pop” represents the tearing of tissue that is not directly attached to the graft? But, for the unlucky ones, the story is different. When a scar is allowed to heal unchecked and unguided, it adheres to anything upon which it can find a foothold — including, in many cases, the tender new tendon graft. If the scar happens to anchor tightly to the graft site, when the athlete begins adding the stress of throwing, it could cause the disorganized, randomly-oriented repair to explode into the “grenade” scene described by Dr. Eaton.
I believe we could be making a colossal mistake by eliminating all valgus stress and by avoiding any movements that mimic throwing in the early stages of rehab. Our efforts to protect the surgical repair by practically immobilizing the arm could be setting the stage for tissue failure. Within the limits of repair site integrity, establishing and maintaining scar tissue order should be the first order of business in any legitimate UCLR or Labrum repair rehabilitation. This can only be accomplished through controlled variable movement that adds the low-grade stress necessary to align the newly forming tissue effectively.
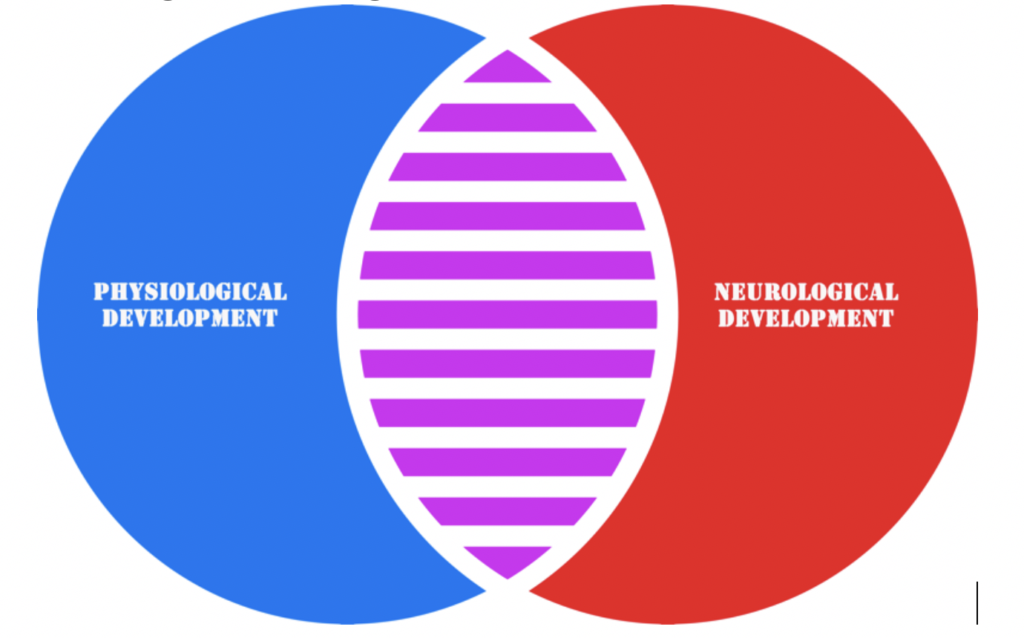
Rehab Programs Must Address Tissue Physiology AND Motor Control Simultaneously
What we’ve talked about so far is the physiology of the process. But, we haven’t yet discussed the impact of the extended rest and protection on motor control and coordination. As Dr. Eaton explained, the scar is an important stabilizer of the post-UCLR elbow. But, the number one stabilizing component of the system is dynamic motor control. The passive restraints provided by to the labrum and the UCL are the last line of defense. If your labrum and UCL are the points of primary stability, you’re probably already in trouble. The timing, sequencing, and synergy of surrounding musculature must be optimized to attenuate the stress on the UCL and labrum. Just like any other physiological system, the motor control system adapts precisely to the neuromuscular coordination demands it experiences. Lack of demand equals no adaptation. No coordinative demand equals no motor control. And, according to the SAID principle of rehab and training (Specific Adaptation to an Imposed Demand), the system will adapt directly in accordance with the stresses under which it is placed. When rehabilitating our players, the training experience we choose in every phase of recovery must keep tissue integrity paramount, but that experience must also be specific to the adaptation we are trying to elicit. It must mimic, as closely as possible, the parameters of the conditions our players will face in life and when they return to games.
And, one thing we know for sure is that the stress our players must handle in life and in games will be largely unpredictable. To bulletproof our players against the variability and unpredictability they will eventually face, we must introduce incrementally increasing variability, or unpredictability as early and as safely as possible. When introduced slowly and within the limits of tissue integrity, variability will allow physiological and neurological self-organization of coordinated movement to progress simultaneously.

As healing tissue organizes to withstand stress, it presents new coordinative demands. If we help an athlete develop the capacity to handle a given level of physiological stress, but we don’t also incorporate a motor control plan to keep the movement within the boundaries of safety, yet highly resistant to perturbation, we may be dooming them to failure. Connective tissue, whether healthy or healing, must remain physiologically and neurologically organized at all times.

Return-to-throwing protocols that feature mindless adherence to a pre-scripted regimen of throws ignore many of the factors that contributed to the injury in the first place. It’s vital that we employ a thorough multi-faceted assessment process to identify possible contributors. When deficits are noted, we must incorporate training strategies that influence the athlete to achieve efficiency in all 6 types of contributors to sub-par performance and/or pain.
Rehab Programs Must Be Individualized
“One-size-fits-all fits none.” Training plans must be customized to meet the individual needs of every player, and they must be changed as the condition of the athlete changes. Cookie-cutter recipes for rehab will never be adequate for optimizing outcomes. Rehabilitation protocols should should illuminate overall principles and goals, and they should serve as general guides and . But, they should never be viewed as a governor, and they should never replace or limit the sound professional judgment of an experienced and qualified rehabilitation professional or coach.
Additionally, rehab protocols must be remain contemporary and should be changed and updated with the times.
As new information emerges, our approach to rehabilitation should be modified to reflect the most current training concepts. The current approach to rehabilitating injured throwing athletes is based on a program first introduced in the late 1970s. It is antiquated, ineffective and it stifles the creativity and adjustability necessary to achieve consistently positive outcomes.
We believe it is time for a change.
Our recommendations:
- As soon as intra-operative bleeding is curtailed, remove the bulky dressing and eliminate all post-operative icing.
- Start Marc Pro to assist with exudate evacuation, (for as often and as long as you can) thereby creating a more optimal healing environment.
- Add multidimensional low amplitude oscillations and gradually increase intensity as early as tissue integrity will allow.
- Begin early progressions of functional range of motion including active movements in multiple planes and in “throwing-like” exercises performed within pain limits. High-frequency, low-intensity motion should begin the day after surgery.
- Challenge all non-throwing arm attractors with light perturbations, variability and unpredictable loads ASAP after surgery.
- Incrementally challenge the Throwing Arm Attractor as soon as tissue integrity allows. use low grade
- Integrate variability/unpredictability early in the rehab process and influence more efficient movement patterns using self-organization techniques.
- Utilize technology to measure stress and fatigue objectively, but teach our patients/players to become intimately familiar with how their arms feel. Let that be the ultimate guide for the process.
- Design return to throwing and rehabilitative processes that allow each player to modulate his training experience based on how his arm and body feel on any given day, at any given moment (see Jaeger-Sullivan Return to Throwing Manual).
- Use pain as the boundary marker, but allow each athlete progress as quickly, or as slowly as his body prefers. Be prepared to adjust the plan daily based on each athlete’s subjective report on the status of pain, weakness, tightness, fatigue, etc.
Before publishing this article, I shared it with three trusted friends and colleagues, ARMory Director of Player Development, Wes McGuire , Dr. Stephen Osterer, and Alan Jaeger. They added some important thoughts.
Wes McGuire: “We need to reconsider the value and potential corruptive nature of the initial throws in the traditional return to throwing protocol. Having experienced my own UCL recovery in high school, I am certain that the mechanics of a 50% effort throw are completely alien and might contribute to disconnections later in the rehab process. So many people (me included when I was recovering from a UCLR) develop some degree of ‘The Yips’ during UCL recovery. Could it be that these super-low intensity post surgical throws are offering disrupted sensory information that result in bad movement patterns?”
Dr. Stephen Osterer: “Something that would interest me in writing would be going into a bit more depth on how tissue loading directs directionality and composition of tissue, how all connective tissue is interconnected (van der Waals continuum), collagen deposition & type, and provide just a bit more insight into the importance of loading in general.
I’d love to explore the concept of how variability in stress can lead to robustness, and that robustness is critical to resiliency – all from a rehabilitation standpoint. Consider how the majority of ‘return to throw’ is repetitive drill work, repetitive exercises, etc. Narrow bandwidth of solutions = narrow bandwidth of tissue resiliency. This includes restoring joint range of motion (and proprioception) to increase the space of the elemental variables (a la UCM hypothesis) & that variability of load within that space may enhance the size of that space.
Another interesting topic would be inducing fatigue on purpose to drive physiological adaptation, but in controlled frequency and duration.
Interested in the pain science component?
The effect of fear and tight coupling / freezing of degrees of freedom and how variability and novelty in task ‘free’ that?
Kinesiophobia would be an interesting avenue to walk down – not sure that I’ve found or read much about it elsewhere in baseball.”
_________________________________________________________________________________________________________________
When the current universal UCLR protocol was written, it was still ok for guys to smoke cigarettes in the dugout. I think it’s time to take another look. I think it’s time for a change.
Get started by calling, our CFO/COO Amy, at 866-787-4533.
We’ll see you at The ARMory.

Randy Sullivan, MPT, CSCS CEO, Florida Baseball ARMory